Appearance
Chapter 9: Bone Medications—When and How They Help
9
Sometimes lifestyle changes aren't enough. When fracture risk is high, medications can dramatically reduce your chances of breaking a bone. Let's demystify how these drugs work, when they're used, and what to expect.
Two Types of Bone Drugs
All osteoporosis medications fall into two camps:

The Stoppers (Antiresorptives)
These slow down bone breakdown:
- Make the demolition crew (osteoclasts) less active
- Let your bone builders catch up
- Examples: bisphosphonates, denosumab
The Builders (Anabolics)
These speed up bone building:
- Stimulate construction workers (osteoblasts)
- Actually build NEW bone
- Examples: teriparatide, abaloparatide, romosozumab
The Stoppers: Bisphosphonates
Names you might hear: Alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), zoledronic acid (Reclast)
These have been around since the 1990s and are the most commonly prescribed bone drugs.
How they work:
- You take the medication
- It binds tightly to your bone mineral
- When an osteoclast (bone-eating cell) comes along and starts breaking down that bone, it swallows the drug too
- The drug disrupts the osteoclast's internal machinery
- The osteoclast dies or stops working
- Result: Less bone breakdown
What you can expect:
- 40-70% reduction in spine fractures
- 30-50% reduction in hip fractures
- Bone density increases about 4-8% over 3 years
How they're taken:
| Drug | How Often |
|---|---|
| Alendronate | Weekly pill |
| Risedronate | Weekly or monthly pill |
| Ibandronate | Monthly pill or quarterly IV |
| Zoledronic acid | Yearly IV infusion |
Taking Oral Bisphosphonates Correctly
This part is important—these pills are picky:
- Take first thing in the morning on an empty stomach
- Swallow with a full glass of plain water (not juice, coffee, or mineral water)
- Stay upright for 30-60 minutes afterward (don't lie back down!)
- Don't eat or drink anything else for 30-60 minutes
Why so fussy? These pills are barely absorbed (only about 1%!), and food or other drinks block absorption even more. The upright position prevents the pill from irritating your esophagus.
Side effects:
- Stomach or esophagus irritation (oral pills)
- Flu-like symptoms after IV infusion (usually just the first dose)
- Rare: Jaw bone problems (osteonecrosis of the jaw)
- Rare: Unusual thigh fractures (atypical femoral fractures)
Understanding the Rare but Serious Side Effects
These rare complications both stem from the same root cause: severely suppressed bone turnover.
Jaw osteonecrosis—why the jaw? Your jaw has bone turnover about 10x higher than other bones because of constant stress from chewing and the presence of teeth. Bisphosphonates accumulate preferentially where turnover is high—so the jaw gets a concentrated dose.
If an infection occurs (say, after a tooth extraction), normal bone would remodel away the infected tissue and replace it with healthy bone. But with turnover suppressed, the damaged and infected bone can't be removed. The result: dead bone that doesn't heal. This is why dentists ask about bisphosphonate use before extractions.
Atypical femoral fractures—what's happening? Normal daily activity causes tiny microcracks in bone. Normally, osteoclasts detect and remove this microdamage, and osteoblasts fill it in with fresh bone. With bisphosphonates suppressing this process, microdamage accumulates over years.
The lateral (outer) femur shaft experiences the most bending stress. With microdamage piling up and no repair happening, the bone eventually fails—often with minimal trauma. These fractures are different from typical hip fractures: they occur in the shaft, not the neck, and often show stress fracture signs beforehand (thigh pain for weeks/months).
Putting risk in perspective:
- These complications are rare (roughly 1-5 per 10,000 patient-years for atypical fractures)
- Risk increases with duration of use (hence drug holidays)
- The fractures PREVENTED by bisphosphonates far outnumber those caused
- But this is why long-term use requires monitoring and periodic reassessment
Drug holidays: After 3-5 years, your doctor might suggest a break. The drug stays in your bones and keeps working for a while even after you stop, while allowing some bone turnover to resume and clear accumulated microdamage.
The Stoppers: Denosumab (Prolia)
This is a newer type of stopper that works differently.
How it works: Remember RANKL—the signal that tells osteoclasts to activate? Denosumab blocks that signal, so osteoclasts never get the message to start breaking down bone.
What you can expect:
- Very powerful suppression of bone breakdown
- Bone density keeps increasing year after year (unlike bisphosphonates which plateau)
- 68% reduction in spine fractures, 40% reduction in hip fractures
How it's taken:
- Injection under the skin every 6 months
- Given at a doctor's office or self-administered at home
- No stomach issues (not a pill!)
Critical Warning: Don't Just Stop Denosumab
This is really important. When denosumab wears off:
- Your osteoclasts come back with a vengeance
- Bone breakdown accelerates dramatically (a "rebound" effect)
- You can lose all the bone you gained—and more
- Multiple spine fractures have occurred in people who stopped without a plan
If you start denosumab, plan to:
- Stay on it long-term, OR
- Transition carefully to a bisphosphonate when stopping
- Never just stop without discussing with your doctor
The Builders: Teriparatide (Forteo)
Now we get to the bone BUILDERS. These are more powerful but also more complex.
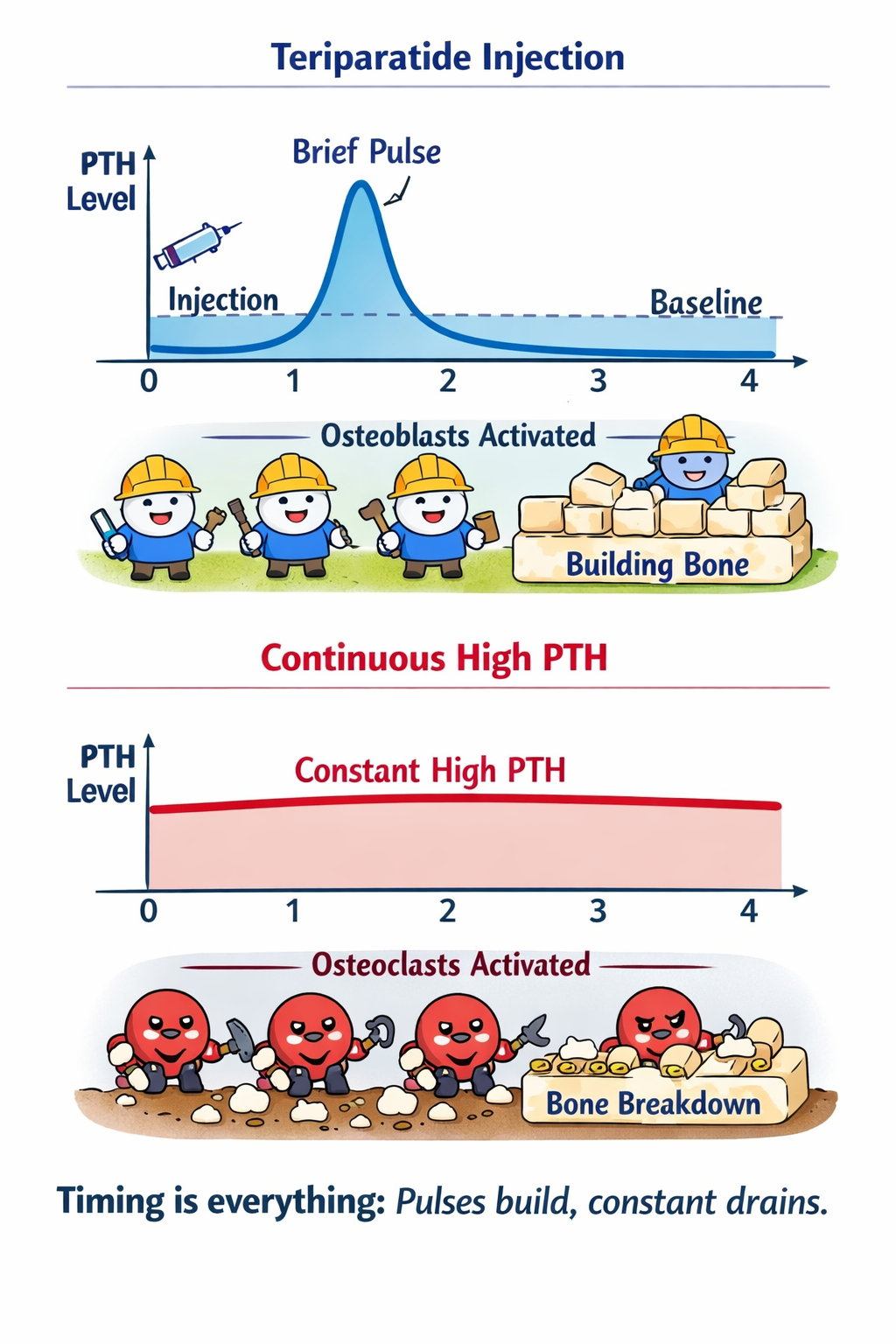
What it is: A piece of parathyroid hormone (PTH)
Wait, doesn't PTH break down bone? Yes, when it's constantly high. But here's the twist: brief daily pulses of PTH actually stimulate bone building. (This is the PTH paradox we covered in Chapter 3.)
How it works:
- You inject a small dose each morning
- PTH spikes briefly then returns to normal
- This pulse pattern activates bone-building cells
- Net result: New bone is formed
What you can expect:
- 9-13% spine density increase over 2 years
- 65% reduction in spine fractures
What happens to bone markers:
- P1NP (formation) rises dramatically—typically doubles within 3 months, peaks at 150-300% above baseline by 6-12 months
- CTX (breakdown) also rises, but more modestly—around 50-80% increase
- Both markers rising reflects the "anabolic window"—bone building outpaces breakdown
- A rise of >20 ng/mL in P1NP within the first few months indicates you're responding to the drug
How it's taken:
- Daily self-injection (tiny needle, like insulin)
- Take in the morning (can cause slight dizziness)
- Usually 2 years of treatment (loses effectiveness after a while)
Monitor Your Vitamin D Levels
PTH—whether natural or from teriparatide—stimulates the kidney enzyme that converts inactive vitamin D (25-hydroxyvitamin D) into active vitamin D (1,25-dihydroxyvitamin D).
Studies show that teriparatide treatment:
- Increases active vitamin D by 20-30% within the first month
- Decreases inactive vitamin D stores by ~19% over 12 months (since more is being converted)
This means your blood vitamin D level (the inactive form doctors measure) can drop during treatment, even if you're taking supplements. Your doctor should monitor 25-hydroxyvitamin D periodically, especially if you started with borderline levels, have low sun exposure, or are overweight. Adequate vitamin D supplementation during treatment is important.
The Cortical vs. Trabecular Paradox
Teriparatide affects different types of bone in different ways—and understanding this explains some confusing scan results.
Trabecular bone (the inner spongy part, dominant in the spine):
- Responds quickly and dramatically
- BMD increases are visible within months
- This is where you see the big gains (+9-13% at the spine)
Cortical bone (the dense outer shell, dominant at the hip and wrist):
- Initially, BMD may actually decrease slightly
- This happens because teriparatide increases cortical porosity (temporary holes from active remodeling)
- At the same time, new bone is being added to the outer surface (periosteal apposition)
Why does cortical BMD drop but strength increase?
Here's the key insight from research: while the inside of cortical bone becomes temporarily more porous, the outside is expanding through periosteal bone formation. The bone is getting wider.
Remember from Chapter 5: bone strength scales with diameter to the fourth power. A slightly wider bone with some internal porosity can actually be stronger than a narrower, denser bone.
| Time on Teriparatide | Cortical BMD | Cortical Thickness | Bone Strength |
|---|---|---|---|
| 6 months | Decreases | Increasing | Improving |
| 12-18 months | Stabilizes | Increased | Significantly better |
| 24 months | May improve | Increased | Much stronger |
The temporary porosity eventually fills in with new, healthy bone. Studies show these "voids" are active remodeling sites, not structural damage.
Don't Panic at Early Scans
If your hip or wrist BMD dips in the first 6-12 months of teriparatide, this is expected. It doesn't mean the drug isn't working—it means bone geometry is being restructured. Strength improvements are happening even when the scan looks worse.
After stopping: You MUST follow up with a "stopper" medication (like a bisphosphonate or denosumab). Otherwise, you'll lose what you gained.
The Builders: Abaloparatide (Tymlos)
Similar to teriparatide—another daily injection that pulses a PTH-like signal.
Differences:
- May work slightly faster at the hip
- Same 2-year limit
- Also requires follow-up with a stopper medication
The Builder/Stopper Combo: Romosozumab (Evenity)
This is the newest and most powerful bone drug.
How it works: Remember sclerostin—the signal that puts the brakes on bone building? Romosozumab blocks sclerostin, which:
- Removes the brake on bone building (more formation!)
- Also reduces bone breakdown
- Dual action = biggest bone density gains
What you can expect:
- Largest BMD increases of any osteoporosis medication
- 13-15% spine increase in just 12 months
- Better fracture prevention than standard treatment
How it's taken:
- Two injections under the skin each month
- 12-month course only
- Must be followed by a stopper medication
Heart Health Caution
Romosozumab carries a warning about cardiovascular events. In one study, there were slightly more heart attacks and strokes compared to another medication.
Not recommended if you've had:
- Recent heart attack
- Recent stroke
- Significant heart disease risk
Talk to your doctor about whether it's right for you.
The Golden Rule: Builders First
Here's something crucial that many doctors unfortunately get wrong:
If you're going to use a bone-building drug, use it FIRST—before bisphosphonates.
Why? Bisphosphonates stick around in your bones for years. If you take them first, they dampen the bone remodeling that builder drugs need to work effectively.
If you start with bisphosphonates:
- The builder drug won't work as well
- You've wasted the best intervention opportunity
- Some bone density potential is permanently lost
When to Use What
| Situation | Consider |
|---|---|
| Moderate risk, never fractured | Bisphosphonate (stopper) |
| Very high risk or very low BMD | Builder first, then stopper |
| Previous spine fractures | Builder first, then stopper |
| On steroids long-term | Consider builder (teriparatide) |
| Kidney problems | Denosumab (doesn't affect kidneys) |
| Heart disease concerns | Avoid romosozumab; use alternatives |
Monitoring Treatment
Your doctor will track whether the medication is working:
Blood tests:
- CTX (breakdown marker) should drop on stoppers
- P1NP (building marker) should rise on builders
- Checked at baseline and 3-6 months later
Bone density scans:
- Typically repeated every 1-2 years
- Should see improvement or at least stability
- If losing bone despite treatment, something's wrong (adherence? secondary cause?)
Use the Same Machine Every Time
DXA machines have variance between them—different machines can give different readings for the same bones. Even two different technicians on the same machine can produce slightly different results. To accurately track changes from treatment, always get your follow-up scans at the same facility, on the same machine, and ideally with the same technician. Otherwise, you can't tell if a change is real or just measurement variation.
Quick Comparison
| Drug | Type | How Taken | Key Advantage | Key Concern |
|---|---|---|---|---|
| Alendronate | Stopper | Weekly pill | Cheap, proven | Fussy to take |
| Zoledronic acid | Stopper | Yearly IV | Most convenient | Initial flu-like symptoms |
| Denosumab | Stopper | Every 6 mo injection | Keeps working year after year | Must not stop abruptly |
| Teriparatide | Builder | Daily injection | Actually builds new bone | Expensive, 2-year limit |
| Romosozumab | Builder + Stopper | Monthly injections | Biggest gains | Heart warning |
The Bottom Line
When lifestyle isn't enough, medications can dramatically reduce fracture risk—but the order and approach matter.
Key takeaways:
- Stoppers (bisphosphonates, denosumab) slow breakdown
- Builders (teriparatide, abaloparatide, romosozumab) stimulate new bone
- If using a builder, use it FIRST—before bisphosphonates
- Denosumab must not be stopped without a transition plan
- All builder drugs need follow-up with a stopper
- Romosozumab offers the biggest gains but has heart concerns
- Work with your doctor to choose the right approach for your situation
Next up: some final thoughts and key takeaways to remember.
