Appearance
Chapter 4: Sneaky Conditions That Steal Your Bones
4
Sometimes bone loss isn't just "getting older"—there are hidden conditions that quietly steal your bone strength. The good news? Many are treatable once you know they're there. Let's play detective.
The Too-Lean Problem
Remember how body fat makes estrogen? When there's not enough fat, estrogen production drops—and bones pay the price.
This affects more people than you'd think:
- The ultra-fit marathon runner with 6% body fat
- The dedicated athlete who lost her period
- The elderly person who's accidentally lost weight
- Anyone severely restricting calories
It Doesn't Care How Healthy You Look
A person can appear incredibly fit and healthy on the outside while their bones are quietly crumbling. You can't outrun low estrogen—even with all the exercise in the world.
Warning signs to watch for:
- Women: Irregular or missing periods
- Men: Low energy, decreased strength despite training
- Anyone: Stress fractures, slow recovery, fatigue
Rough body fat guidelines (varies by individual):
| Risk Zone | |
|---|---|
| Women | Below ~17-20% body fat |
| Men | Below ~8-10% body fat |

Overactive Parathyroid Glands
Remember PTH from Chapter 3? Sometimes those tiny glands in your neck go haywire and pump out too much PTH constantly. This is called hyperparathyroidism.
What happens:
- PTH tells bones to release calcium non-stop
- Calcium floods into the blood (too much)
- Bones get progressively weaker
- Often, people don't feel symptoms until significant damage is done
Classic symptoms (though many people have none):
- Kidney stones
- Bone pain
- Stomach problems, constipation
- Feeling mentally foggy or depressed
The tell-tale lab finding: High calcium AND high PTH at the same time. Normally, high calcium should make PTH go DOWN. When both are high, something's wrong with the parathyroids.
Celiac Disease: The Hidden Bone Thief
About 1 in 100 people has celiac disease—but many don't know it. When someone with celiac eats gluten (found in wheat, barley, rye), their immune system attacks the small intestine.
How it hurts bones:
- Damaged intestine can't absorb calcium and vitamin D properly
- Body gets inflamed, which accelerates bone breakdown
- May trigger the PTH problems mentioned above
Consider Testing If...
- You have unexplained bone loss, especially if you're young
- Osteoporosis treatments aren't working
- You have other autoimmune conditions (thyroid issues, type 1 diabetes)
- Family members have celiac
- You have digestive symptoms (though many people don't!)
The silver lining: Going gluten-free can actually help restore bone density if caught early enough.
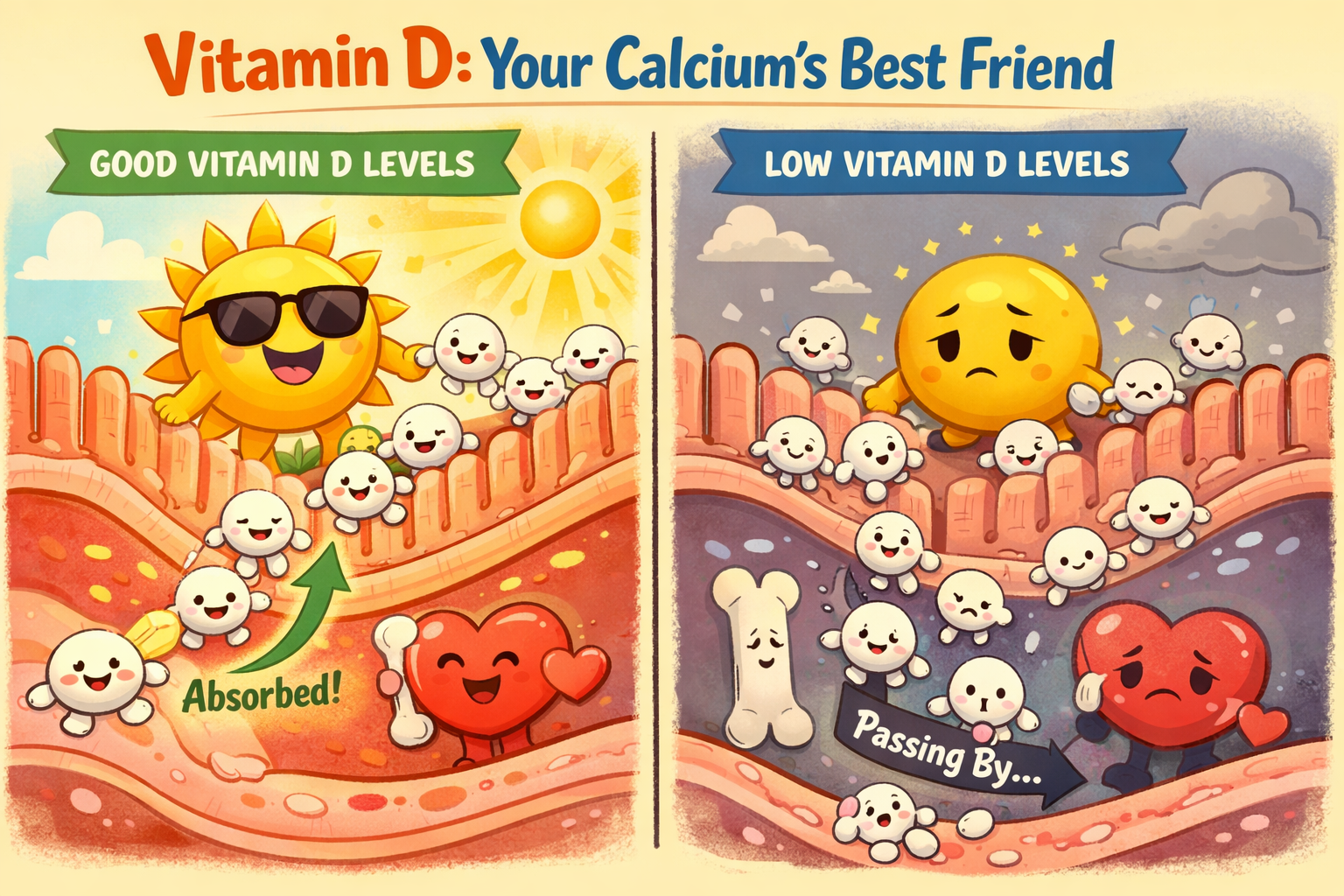
Not Enough Vitamin D
Vitamin D is your calcium helper—without enough, you only absorb 10-15% of the calcium you eat. With good vitamin D levels, you absorb 30-40%.
Why so many people are low:
- Not enough sunlight (office jobs, northern climates, sunscreen)
- Darker skin (melanin blocks vitamin D production)
- Being overweight (fat holds onto vitamin D)
- Digestive issues that affect absorption
- Getting older (skin makes less vitamin D)
What happens when you're deficient:
- Mild deficiency: Body steals calcium from bones to maintain blood levels
- Severe deficiency: Bones can actually soften (a condition called osteomalacia), causing pain and weakness
Good levels to aim for: Blood test (25-OH vitamin D) between 30-70 ng/mL.
Proton Pump Inhibitors (PPIs): The Acid-Blocking Bone Thief
PPIs like omeprazole (Prilosec), esomeprazole (Nexium), and pantoprazole (Protonix) are among the most commonly prescribed medications worldwide. While they're excellent for treating genuine acid-related conditions, long-term use comes with bone health consequences that many people don't know about.
How PPIs hurt calcium absorption:
Stomach acid isn't just for digestion—it's essential for absorbing calcium. Here's why:
- Calcium carbonate needs acid to dissolve. This is the most common and cheapest form of calcium supplement. Without adequate stomach acid, calcium carbonate is poorly absorbed.
- While research is mixed on exactly how much PPIs reduce calcium absorption, long-term use is associated with a 20-30% increased risk of hip fracture
- Over years, this can contribute to weakened bones
Calcium Citrate: The PPI-Friendly Alternative
Unlike calcium carbonate, calcium citrate doesn't require stomach acid to be absorbed. If you're on a PPI and need calcium supplementation, calcium citrate is the smarter choice—though it's typically more expensive and requires taking more pills.
The irony most people don't know about:
Many people taking PPIs for reflux disease believe they have too much stomach acid. The surprising truth? A significant portion of them actually have too little acid—a condition called hypochlorhydria.
Here's the paradox:
- Low stomach acid can cause the same symptoms as high acid: heartburn, reflux, bloating
- Why? Without enough acid, food sits in the stomach too long, ferments, and creates pressure that pushes stomach contents upward
- Taking a PPI makes this underlying problem even worse while masking the symptoms
- Meanwhile, calcium absorption drops further, and bones quietly suffer
Who's at risk for low stomach acid?
- Adults over 50 (stomach acid production naturally decreases with age)
- People who've been on PPIs for years
- Those with autoimmune conditions
- People with H. pylori infection
Testing and addressing low stomach acid:
If you suspect low stomach acid, there are ways to confirm it:
- Heidelberg test — the gold standard, where you swallow a small capsule that measures stomach pH directly
- Gastrin blood test — elevated fasting gastrin can indicate low acid production
- Baking soda test — a simple at-home screening (not definitive): drink 1/4 tsp baking soda in water on an empty stomach; if you don't burp within 3-5 minutes, low acid is possible
If low stomach acid is confirmed, betaine HCL supplements (taken with protein-containing meals) can make a significant difference. They provide the acid your stomach isn't producing, helping you properly digest protein and absorb minerals like calcium, magnesium, and zinc. Many older adults who add betaine HCL report dramatically improved digestion.
Digestive enzymes (proteases, lipases, amylases) can also help, especially if you experience bloating, gas, or feel like food "sits" in your stomach. These don't replace stomach acid but assist with the breakdown process. Some people benefit from combination products that include both betaine HCL and digestive enzymes.
The PPI Trap
Many people get stuck in a cycle: they take PPIs for reflux symptoms, the symptoms improve, so they stay on them indefinitely. But the underlying cause—sometimes low acid, not high—never gets addressed. Years later, they have weakened bones and a dependency on medications they may not have needed in the first place.
If you're on a PPI long-term:
- Ask your doctor if you really still need it—many people were put on PPIs for short-term issues that resolved
- Consider trying to step down to a lower dose or switch to an H2 blocker (less impact on calcium)
- If you must stay on a PPI, switch to calcium citrate rather than calcium carbonate
- Make sure your vitamin D is adequate (you need it to absorb whatever calcium you can)
- Get your bone density checked if you've been on PPIs for several years
(Cortico)Steroid Medications (not to be confused with anabolic steroids taken by bodybuilders/athletes)
If you've been on prednisone or similar steroids for conditions like asthma, arthritis, or autoimmune diseases, your bones may be at risk.
What are they:
- They mimic your body's natural hormone called cortisol, which is a catabolic hormone (catabolic means it breaks down stuff)
How steroids hurt bones:
- Slow down the bone builders
- Speed up bone breakdown
- Reduce calcium absorption from food
- Weaken muscles (less pull on bones)
The scary part: Bone loss starts within months and is fastest in the first year. Even low doses can increase fracture risk.
If you're on long-term steroids:
- Get a baseline bone density scan
- Make sure vitamin D and calcium are adequate
- Talk to your doctor about bone-protective medications
- Use the lowest effective steroid dose
Thyroid Problems
Both an overactive and underactive thyroid can affect bones, but overactive is more concerning:
Hyperthyroidism (overactive) speeds up bone remodeling—but breaking outpaces building, leading to net loss.
Common causes:
- Graves' disease
- Thyroid nodules
- Taking too much thyroid medication
Even mildly elevated thyroid function can affect bones over time.
Inflammatory Conditions
Chronic inflammation is bad news for bones. Conditions like rheumatoid arthritis, inflammatory bowel disease, and lupus can cause bone loss through:
- Inflammatory signals that boost bone breakdown
- Medications used to treat them (especially steroids)
- Reduced activity during flares
Sleep Apnea
Here's one most people don't expect: obstructive sleep apnea is associated with lower bone density and higher osteoporosis risk.
The numbers: A meta-analysis of over 113,000 subjects found that people with sleep apnea have roughly twice the odds of developing osteoporosis compared to those without. Lumbar spine BMD and T-scores were significantly lower in sleep apnea patients.
How it hurts bones:
- Intermittent hypoxia (repeated drops in oxygen) promotes osteoclast formation while suppressing osteoblasts
- Vitamin D disruption—sleep apnea may lead to vitamin D deficiency and secondary hyperparathyroidism
- Severity matters: the worse the apnea, the greater the bone loss
The good news: Treating sleep apnea effectively (with CPAP or other interventions) may help reduce osteoporosis risk. If you snore heavily, wake up tired, or have been told you stop breathing at night, getting evaluated could benefit more than just your sleep.
Osteogenesis Imperfecta (Brittle Bone Disease)
Unlike the other conditions in this chapter, osteogenesis imperfecta (OI) is genetic—you're born with it. But it's worth knowing about, especially if unexplained fractures run in a family.
What it is: A group of genetic disorders (at least 19 types) caused by defects in collagen production. Remember, collagen is the flexible scaffolding that gives bones their toughness. Without proper collagen, bones become brittle and break easily—sometimes from minimal or no trauma.
How common: About 1 in 15,000-20,000 people. Rare, but not as rare as you might think.
The spectrum:
- Type I (mildest, most common): Normal-shaped bones that break more easily than they should. Blue-tinted whites of the eyes. May have hearing loss as adults.
- Type II (most severe): Often fatal at or shortly after birth.
- Types III-IV: Frequent fractures, abnormally shaped bones, short stature, curved spine, brittle teeth.
Red flags that might suggest OI:
- Multiple fractures from minor injuries, especially in childhood
- Family history of "fragile bones" or unexplained fractures
- Blue or gray sclera (whites of the eyes)
- Early hearing loss
- Teeth that chip or break easily
Treatment: There's no cure, but bisphosphonates can help strengthen bones and reduce fractures. Physical therapy, careful fracture management, and lifestyle modifications (avoiding smoking, steroids, excessive alcohol) are also important.
When to Dig Deeper
Consider asking your doctor about testing if:
| Situation | Possible Cause |
|---|---|
| Very low bone density in a young person | Celiac, malabsorption, genetic condition |
| High calcium on blood tests | Hyperparathyroidism |
| Treatment isn't working | Hidden secondary cause |
| Unexplained weight loss | Malabsorption, other illness |
| Much worse than expected for your age | Something beyond normal aging |
Basic screening tests:
- Blood count and metabolic panel
- Vitamin D level
- PTH level
- Thyroid function (TSH)
- Celiac antibodies
The Bottom Line
Many treatable conditions silently steal bone. Finding and fixing these is often more effective than just taking osteoporosis medications.
Key points:
- Being too lean causes estrogen deficiency in both sexes
- Overactive parathyroids can drain calcium from bones
- Celiac disease is common and often undiagnosed
- Vitamin D deficiency is widespread and easy to fix
- Long-term PPI use impairs calcium absorption—and many "acid reflux" sufferers actually have too little acid, not too much
- Steroid medications are hard on bones
- Sleep apnea doubles osteoporosis risk through hypoxia and vitamin D disruption
- Osteogenesis imperfecta is a genetic collagen disorder causing brittle bones from birth
- Always look for underlying causes, especially in younger people
Next up: we'll explore why your teenage years matter so much for lifelong bone health.
